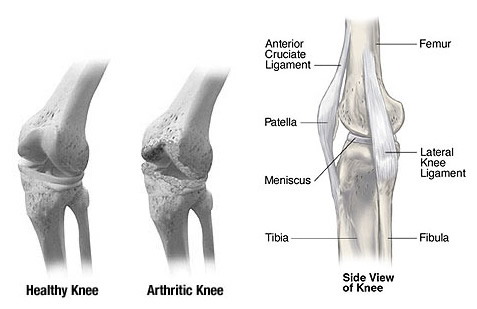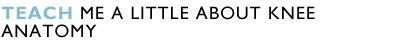
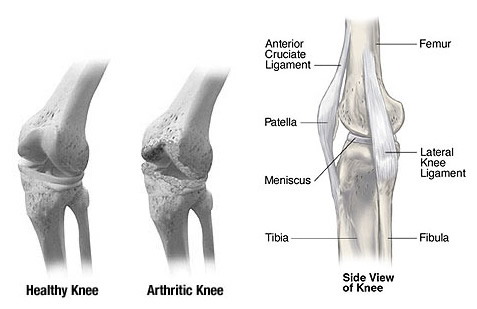
Your knee joint is made up of three bones. Your thigh bone (femur) sits on top of your shin bone (tibia). When you bend or straighten your knee, the rounded end of your thigh bone rolls and glides across the relatively flat upper surface of your shin bone. The third bone is often called the kneecap (patella), which is attached to the muscles that allow you to straighten your knee. Your kneecap provides leverage that reduces strain on these muscles.
BONES
The bones of the knee are the femur (thigh bone), tibia (shin bone) and patella (kneecap). The femur and tibia meet to form a hinge with the patella in front of these two bones protecting the joint. The patella slides up and down in a groove
in the femur (the femoral groove) as the knee is bent and straightened.
LIGAMENTS
Ligaments hold the knee together and give it stability. The medial (inner) collateral ligament (MCL) and outer (lateral) collateral ligament (LCL) limit sideways motion of the knee. The posterior and anterior cruciate ligaments (PCL and ACL)
limit backward and forward motion of the knee bones, keeping them stable.
CARTILAGE
Two structures known as menisci sit between the femur and the tibia and act as cushions or shock absorbers for the knee. A torn meniscus is often referred to as "torn cartilage." Menisci are one of two types of cartilage in the knee. The
other type, articular cartilage, is a smooth and very slick material that covers the end of the femur, the femoral groove, the top of the tibia and the underside of the patella. This articular cartilage allows the bones to move smoothly.
TENDONS
Tendons connect muscle to knee. The quadriceps muscles on the front of the thigh are connected to the top of the patella by the quadriceps tendon, which covers the patella and becomes the patellar tendon. The patellar tendon then attaches to the front of the tibia. The hamstring muscles in the back of the leg attach to the tibia at the back of the knee. The quadriceps muscles straighten the knee and the hamstring muscles bend the knee.
Bones, ligaments, cartilage and tendons all work together to build a healthy knee.
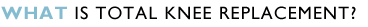
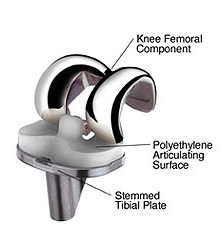
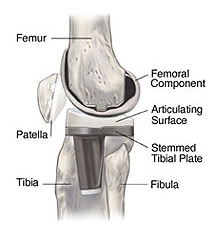
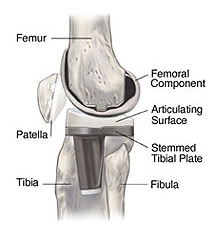
In total knee replacement surgery, the parts of the bones that rub together are resurfaced with metal and plastic implants. Using special, precision instruments, your surgeon will typically remove the damaged surfaces of all three bones. The replacement surfaces will then be fixed into place.
The surface of the femur is replaced with a rounded metal component that comes very close to matching the curve of your natural bone. The surface of the tibia is replaced with a smooth plastic component. This flat metal component holds a smooth plastic piece made of ultra-high-molecular-weight polyethylene plastic that serves as the cartilage. The undersurface of the kneecap may also be replaced with an implant made of the same polyethylene plastic.
If you and your surgeon decide that total knee replacement is right for you, a date will be scheduled for your surgery. Several things may be necessary to prepare for surgery. For example, your surgeon might ask you to have a physical examination by an intern or your regular doctor.
Because blood transfusions are likely to be needed during your surgery, you may want to donate one unit of your own blood, or possibly two units if your surgeon feels it is needed. All preparations for surgery should be discussed with your surgeon.
On the day of surgery, a small tube (intravenous line) will be inserted into your arm. This tube will be used to administer antibiotics and other medication during your surgery. You will then be taken to the operating room and given anaesthesia. After the anaesthesia takes effect, your knee will be scrubbed and sterilized with a special solution.
The surgery will begin with an incision over the knee that will expose the joint. When the bones are fully visible to the surgeon, special, precision guides and instruments are used to remove the damaged surfaces and shape the ends of the bones to accept the implants.
The implants are then secured to the bones. It might also be necessary to adjust the ligaments that surround the knee in order to achieve the best possible knee function. When the surgeon is satisfied with the fit and function of the implants, the incision will be closed.
A special drain may be inserted into the wound to drain the fluids that naturally develop at the surgical site. A sterile bandage will then be applied, and you will be taken to the recovery room, where you will be closely monitored. Your surgery will likely take between one and three hours, depending on your individual circumstances.
As your anaesthesia wears off, you will slowly regain consciousness. A nurse will be with you, and may encourage you to cough or breath deeply to help clear your lungs. You will also be given pain medication. When you are fully awake, you will be taken to your hospital room. Your knee will remain swollen and tender for a few days.
When you are back in your hospital room, you will begin a rehabilitation programme that will help you regain strength, balance, and range of movement in your knee. This programme will be designed specifically for you. It may include a machine, called a continuous passive motion machine that automatically moves your leg to help reduce stiffness.
Your physical therapist will help you perform appropriate exercises. About 24 hours after surgery, you will probably be asked to stand. Within the next 24 hours, you will probably begin to walk a few steps with the help of a walker. You will be discharged as soon as your surgeon determined that you have recovered sufficiently. You can expect to stay in the hospital for about three days after your surgery. You may or may not be transferred to a rehabilitation facility for a few more days, as determined by your surgeon. Your bandages and sutures will usually be removed before you leave the hospital. At home, you will need to continue your exercises. Your physiotherapist will instruct you about proper home care, and may continue to work with you.

Within six weeks after surgery, most patients are able to walk with a cane. You will probably feel well enough to drive a car within seven to eight weeks after surgery.
In most cases, successful joint replacement surgery will relieve your pain and stiffness, and allow you to resume many of your normal daily activities. But even after you have fully recovered from your surgery, you will still have some restrictions. Normal daily activities do not include contact sports or activities that put excessive strain on your joints. Although your artificial joint can be replaced, a second implant is seldom as effective as the first.
Longevity of the prosthetic knee varies from patient to patient. It depends on many factors, such as a patient's physical condition, activity level, and weight, as well as the accuracy of implant placement during surgery. It is useful to keep in mind that prosthetic joints are not as strong or durable as a natural, healthy joint, and there is no guarantee that a prosthetic joint will last the rest of a patient's life.
Today, total knee replacement has become a common and predictable procedure. Many patients enjoy relief from pain and improved function, compared to their status before surgery. As a result, some patients may have unrealistic expectations about what the prosthetic knee can do and how much activity it can withstand. As with any mechanical joint, the knee components move against each other. Natural fluid in the joint space, called synovial fluid, helps to lubricate the implants just as it lubricates the bones and cartilage in a natural joint. Still, the prosthetic components do wear as they roll and slide against each other during movement. As with car tires or brake pads, the rate of wear depends partly on how the knee joint is used. Activities that place a lot of stress on the joint implants, as may be the case with heavier and more active patients, may reduce the service life of the prosthesis. Implant loosening and wear on the plastic portions of the implant can lead to the necessity for revision surgery to replace the worn components, or all of the components. Your doctor will be in the best position to discuss these issues with you, taking into account your particular clinical circumstances, the type of implants used, and your post-surgical lifestyle.
Talk with your doctor about the following points, and how they might affect the longevity and success of your knee replacement:
- Avoiding repetitive heavy lifting
- Avoiding excessive stair climbing
- Maintaining appropriate weight
- Staying healthy and active
- Avoiding "impact loading" sports such as jogging, downhill skiing and high impact aerobics
- Consulting your surgeon before beginning any new sport or activity
- Thinking before you move
- Avoiding any physical activities involving quick stop-start motion, twisting or impact stresses
- Avoiding excessive bending when weight bearing, like climbing steep stairs
- Not lifting or pushing heavy objects
- Not kneeling
- Avoiding low seating surfaces and chairs.
|